Atopic Dermatitis is a common skin disease in childhood and effects many adults too. It’s typically associated with dry, red and itchy skin and can have a significant physical and psychological impact on those whose lives it touches. While there is no known cure, effective skincare has been proven to relieve symptoms and keep skin calmer for longer.
This article gives a general introduction to Atopic Dermatitis. It explains what it is and how it effects people. We examine the possible causes and triggers and make some suggestions about how to soothe flare-ups, alleviate symptoms and care for atopic skin on a daily basis.
What is Atopic Dermatitis?

Atopic Dermatitis – also known as Atopic Eczema – is a non-contagious, chronic (i.e. persistent or long-term) inflammatory and non-contagious skin disease characterized by dry, flaky, itchy (also known as pruritic) and irritable skin which can appear on both the face and the body.
Incidence of Atopic Dermatitis has increased 2- to 3-fold in industrialised nations since the 1970s. 1,2,3 The disease is increasing in prevalence in developing countries too. Atopic Dermatitis is most common in babies and children: approximately 15% to 20% of children globally are thought to suffer with around 90% of all sufferers experiencing symptoms within the first five years of life. 1,2,3
It can persist into adulthood and research indicates that those who have Atopic Dermatitis as children can go on to develop other, related conditions such as asthma and allergic rhinitis4. And, people who never experienced the disease in childhood can also develop it as adults: it is estimated that one in 12 adults suffer from Atopic Dermatitis 5.
Attention Box
I say Dermatitis, you say Eczema
The words are interchangeable and mean the same thing: collective terms for inflammatory changes in the skin. As such, they include many different dermatological diseases.
Atopic Eczema and Atopic Dermatitis are also the same thing (atopic means a hereditary sensitivity to certain allergens).
What are the symptoms of Atopic Dermatitis?


Dryness, itchiness and irritation are all symptoms of atopic skin. In fair-skinned people the affected area of skin is normally reddish in colour and may turn brown. In darker skins, affected skin can become lighter or darker as Atopic Dermatitis affects pigmentation.
Atopic Dermatitis can appear anywhere on the body but the most common locations are: the face (including the area around the eyes), the neck and décolleté, the scalp, elbow folds, knee cavities and hands and feet. You can find out more in Facial Atopic Dermatitis, Atopic Dermatitis on the eyelids, Atopic Dermatitis on the scalp, Atopic Dermatitis on the hands, Atopic Dermatitis on different parts of the body.
The areas affected differ slightly according to age. Read more about that in Atopic Dermatitis and babies, Atopic Dermatitis and children, and Adult Atopic Dermatitis.
What are the different stages of Atopic Dermatitis?
Atopic skin is typified by two phases:
The acute phase
Also known as the ‘active phase’ and often referred to as a ‘flare-up’. This is when atopic skin is at its most irritable:
- Skin feels itchy to intensely itchy. You may experience a burning sensation and it can be sore.
- Skin looks red, dry and flaky. It can be uneven or swollen and may bleed mildly.
The non-acute phase
Between flare-ups there are periods when atopic skin is calmer and less irritable. This non-acute phase is also known as the non-active, interval or flare-up-free phase.
- Skin feels ‘more normal’ (i.e. the symptoms are less irritating)
- Skin looks and feels dry to very dry and may be scaly, slightly flaky and mildly itchy
- Small, healed cracks (from previous flare-ups) may be visible
- Symptoms are similar to those of dry skin (a condition rather than a disease and known as Xerosis). Read more in dry skin in general.
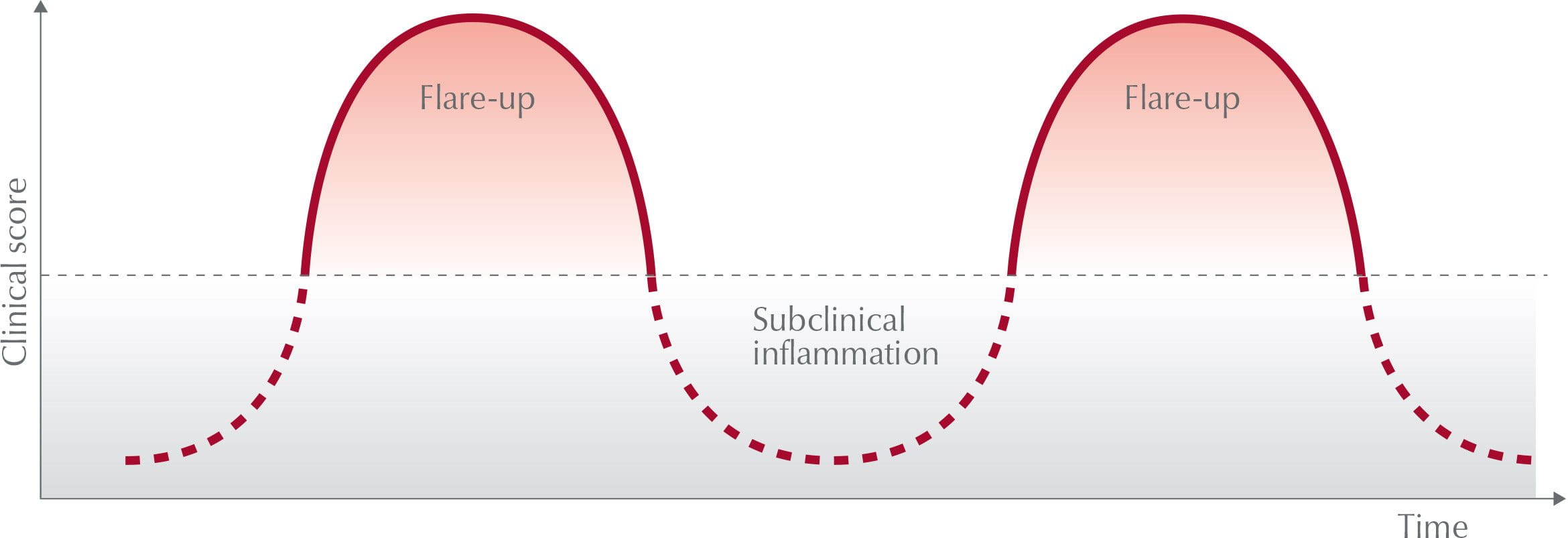
The length of each phase varies greatly on the individual and skincare should be adapted to suit skin’s different needs during each phase.
There is no known cure for Atopic Dermatitis so the primary aim when caring for atopic skin on a daily basis is to prolong the non-acute phase. During a flare-up, the focus is on soothing symptoms and calming skin as quickly as possible.
The Eucerin AtopiControl range has been specially formulated to give skin the care and comfort it needs during each phase.
Can Atopic Dermatitis effect more than your skin?
Living with Atopic Dermatitis, especially during a flare-up, can be distressing and it is known to have a significant impact on quality of life.

In addition to the problems caused by the skin irritation itself, Atopic Dermatitis can lead to physical and psychological issues such as lack of sleep, discrimination, stress and a general lack of self-confidence.
As a result, sufferers often restrict their daily lives by changing what they wear, what they eat, the make-up they choose and the activities they take part in. Relationships can even be affected if the sufferer feels his or her attractiveness is diminished by their symptoms. And, when it’s babies and children that experience Atopic Dermatitis, parents can feel helpless and guilty.
You can read more in How Atopic Dermatitis affects sleep and quality of life, and find out about the specific impact it has on different age groups in in Atopic Dermatitis and babies, Atopic Dermatitis and children, and Adult Atopic Dermatitis.
What causes Atopic Dermatitis?
Atopic Dermatitis is linked to a compromised skin barrier function and an immune disorder.
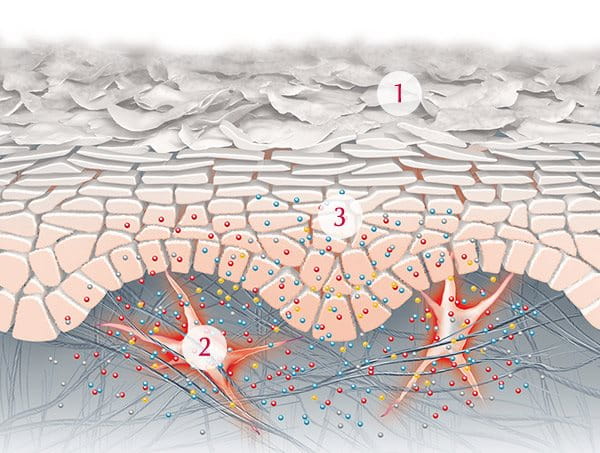
The outermost (epidermal) layers of healthy skin are made up of skin cells (corneocytes) surrounded by a lipid-rich matrix of cholesterol, free fatty acids and ceramide. You can find out more in the structure of skin. In atopic skin, lipid metabolism is abnormal which causes a deficiency in ceramide and leads to transepidermal water loss. 4 This excess loss of water causes skin to dry out which weakens its natural barrier function.
The weakened barrier function in atopic skin is also linked to a deficiency of Filaggrin (a gene responsible for the development of structural proteins that strengthen skin’s barrier function). When skin’s natural barrier function is compromised it is more susceptible to irritation and infection.
Sufferers are also known to have an irregular immune function (known as atopy), which makes their skin more reactive to the environment and susceptible to inflammation.
There are a number of genetic and environmental theories as to why some people develop Atopic Dermatitis and others don’t. These include:


Genetic disposition
There are two major risk factors for the development of Atopic Dermatitis: 1) a genetic defect in the Filaggrin (FLG) gene1,6 and 2) a family history of atopic disease.1,3
Children can inherit a Filaggrin deficiency from affected parents7 and these genetic defects are particularly common among Caucasians.1 Multiple studies have shown that the FLG gene plays a key role in skin barrier function and that mutations of the gene lead to instances of Atopic Dermatitis. When Filaggrin mutations are present the disease is also more severe and persistent.1
Approximately 70% of all Atopic Dermatitis patients have a family history of atopic disease.1,3,8 There is a proven link between the atopic diseases: Atopic Dermatitis, asthma and hay fever. If one or both parents suffer from one of these conditions, there is a chance that their child will develop Atopic Dermatitis. The risk increases proportionally so if both parents have all three conditions, the chance of the child inheriting the disease goes up.
Climate/pollution
Living in a developed country, a city (especially one with higher levels of pollution) or a cold climate seems to increase the risk of Atopic Dermatitis. There is some interesting research on the association between Atopic Dermatitis and climate which you can read more about in Atopic Dermatitis and children.
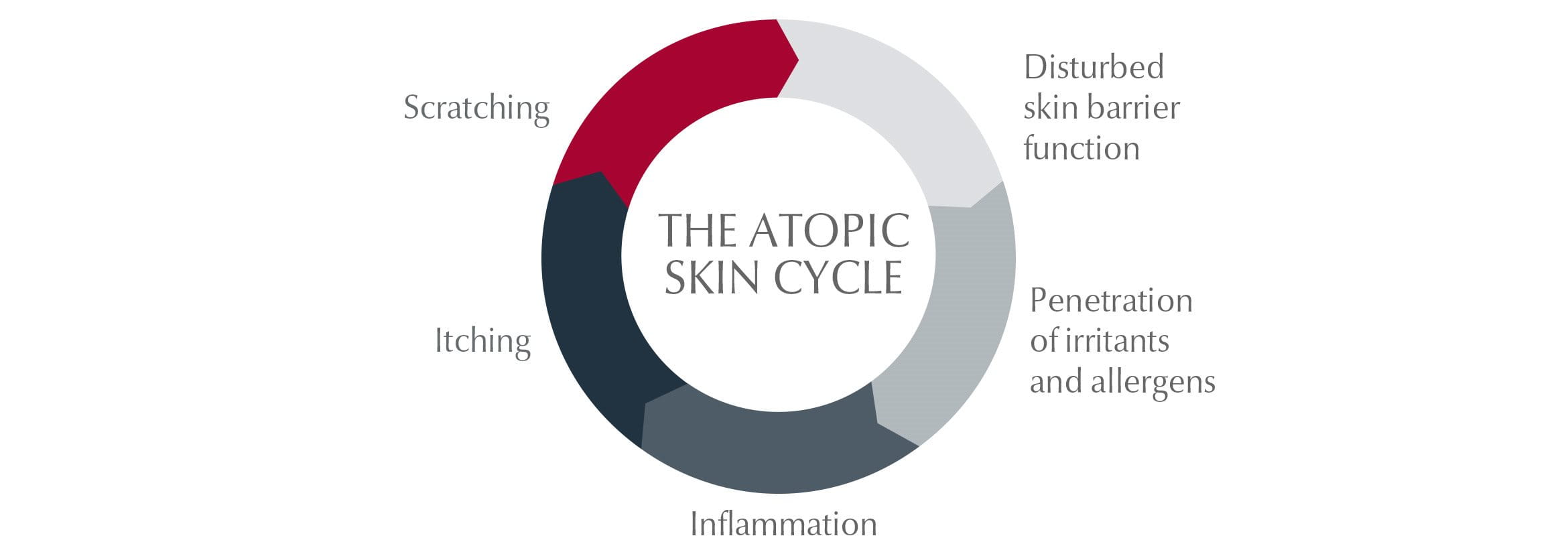
The symptoms of Atopic Dermatitis are also the triggers. Because skin is dry and itchy, sufferers scratch. This scratching damages skin’s protective barrier and a bacteria known as Staphylococcus Aureus is able to multiply and infect skin. This infection causes inflammation and itching which worsens the condition making skin even more irritable and itchy: a vicious circle known as the Atopic Skin Cycle.
The Itch Scratch Cycle
What can trigger a reaction in atopic skin?


There are a number of external influences that can aggravate Atopic Dermatitis and make symptoms worse. These vary from person to person but may include:
- climate and pollution
- sweat
- stress
- allergies
- cigarette smoke
- abrasive or non-breathable fabrics: e.g. wool and nylon
- nickel – a metal found in watches and jewellery
- chemicals such as some washing detergents
- sun: some people find that sun triggers symptoms, for others it improves skin condition
You can find out more about many of these in Identifying and managing flare-ups and factors that influence skin
How to care for skin with Atopic Dermatitis?
A good skincare routine, using products specially formulated for atopic skin, will help to relieve symptoms of Atopic Dermatitis and to give your skin, or your child’s skin, the best chance of staying calmer for longer.


Effective moisturisation: Key to caring for atopic skin is to restore the skin’s natural protective barrier by giving it the moisturisation it needs. Using moisturisers (also known as emollients) daily helps to prevent or delay flare-ups for as long as possible and is known as basic care. Look out for emollients that include proven actives such as:
- Licochalcone A: an extract of liquorice that soothes skin and reduces redness
- Ceramides: which strengthen skin’s barrier function
- Omega-3 and Omega-6: Evening Primrose Oil, Grape Seed Oil and Glycine Soja Oil are all rich sources of these essential fatty acids which soothe and nourish skin while replenishing its protective barrier.
The ingredients are part of the active formula in the Eucerin AtopiControl range of products that has been specially formulated for to care for atopic skin.
Emollients can also help to calm skin when it flares-up. You can find out more in Identifying and managing flare-ups
Medicated ointments: Corticosteroids (such as hydrocortisone) can calm atopic skin during a flare-up. Find out more in Identifying and managing flare-ups. Your doctor will be able to advice on the most appropriate treatment for your skin.
Gentle but thorough cleansing: Cleansing is the important first step in caring for atopic skin. Use gentle but effective cleansers that have been specially formulated to be gentle on atopic skin. Try Eucerin AtopiControl Bath and Shower Oil for your body and Eucerin UltraSENSITIVE Cleansing Lotion for your face.
You can read more about how to give atopic skin the care it needs in how to care for adult atopic skin and how to care for young atopic skin.
Our brand values

We deliver a holistic dermo-cosmetic approach to protect your skin, keep it healthy and radiant.

For over 100 years, we have dedicated ourselves to researching and innovating in the field of skin science. We believe in creating active ingredients and soothing formulas with high tolerability that work to help you live your life better each day.

We work together with leading dermatologist and pharmacist partners around the world to create innovative and effective skincare products they can trust and recommend.
How can I reduce the chances of a flare-up of Atopic Dermatitis?
Because there is no known cure for Atopic Dermatitis, the best way to care for skin is to do everything you can to reduce the chances of it flaring up. Here are some of the things that others have found can make a difference:
Take care when washing skin: Frequent washing in water that is too hot can damage skin’s protective barrier and cause it to try out. Harsh sponges and massage brushes can also stress atopic skin.
Try to wash in lukewarm water, limit bath time, take showers over baths when possible and pat rather than rub skin dry. Take a quick shower as soon as possible after exercise to cool down your body and remove sweat − heat and sweat can trigger flare-ups for some people.
If your work means you need to frequently wash your hands or they are exposed to harsh chemicals then try to limit exposure. You can find out more in Atopic Dermatitis and hands.
Keep cool: Keep room temperatures and humidity low and holiday in cool or moderate climates. This will help to reduce sweating which can trigger irritation and itchiness.
Sun protection: Atopic skin is already dry and the sun causes it to dry out further. Limit your exposure, avoid the peak hours when sun is at its most intense, use protective clothing and apply an appropriate sun protection factor. You can read more in the effects of the sun on sensitive skin.
Wear soft, breathable fabrics: Try to avoid harsh and synthetic fabrics next to your skin. Even wool can causes some people to itch. Some washing detergents can also trigger atopic skin so choose non-biological options to support sensitive skin.
Wear cotton gloves at night: Scratching makes matters worse so if you, or your child, is prone to scratching these can help to reduce damage to the skin.
Make-up: Choose products that have been specially formulated for dry sensitive skin to reduce the chances of irritation.
Try to reduce stress: Relaxation exercises such and yoga and meditation can help reduce stress which is often cited as a trigger for atopic skin, especially by women.
Diet: We’re all different, but some people find that certain foods and drinks trigger their symptoms and milk, eggs, nuts, shellfish and alcohol are frequently cited. Consider keeping a diary to see if there’s anything that causes your or your child’s skin to flare-up, but don’t make significant dietary changes for babies and children before discussing them with your doctor first.
Stop smoking: Cigarette smoke can exacerbate symptoms of Atopic Dermatitis.
You can find out more about many of these in factors that influence skin.
If symptoms persist, or if your skin or your child’s skin is in any way bothering or concerning you, be sure to contact your doctor.
Sources
- Overview of Atopic Dermatitis, Avena-Woods C, Am J Manag Care, 2017 June, Vol. 23, No. 8, Supplement S115-123
- Nutten S. Atopic dermatitis: global epidemiology and risk factors. Ann Nutr Metab. 2015; 66(suppl 1):8-16. Doi: 10.1159/000370220.
- Eichenfield LF, Tom WL, Chamlin SL, et al. Guidelines of care for the management of atopic dermatitis: section 1. Diagnosis and assessment of atopic dermatitis. J Am Acad Dermatol. 2014; 70(2):338-351. doi: 10.1016/j.jaad.2013.10.010.
- Spergel JM. From atopic dermatitis to asthma: the atopic march. Ann Allergy Asthma Immunol. 2010; 105:99–106. doi: 10.1016/j.anai.2009.10.002.
- WebMD
- Sicherer SC, Leung DY. Advances in allergic skin disease, anaphylaxis, and hypersensitivity reactions to foods, drugs, and insects in 2008. J Allergy Clin Immunol. 2009; 123(2):319-327. doi: 10.1016/j. jaci.2008.12.025.
- Comprehensive analysis of the gene encoding filaggrin uncovers prevalent and rare mutations in ichthyosis vulgaris and atopic eczema. Sandilands et al. Nat Genet. 2007 May; 39(5):650-4.
- Wen HJ, Chen PC, Chiang TL, Lin SJ, Chuang YL, Guo YL. Predicting risk for early infantile atopic dermatitis by hereditary and environmental factors. Br J Dermatol. 2009; 161(5):1166-1172. doi: 10.1111/j.1365-2133.2009.09412.x.






